Oral Surgery
Why Do I Need Oral Surgery?
Odds are if you do, it will be for wisdom teeth removal. This is definitely the most common type of oral surgery we do in our office probably because just about every young adult needs it.
We also surgically place dental implants when you need stable support for crowns. And if, upon routine examination, should we find some questionable tissue, cyst or growth, we can easily remove it with our Waterlase® surgical laser, then any needed biopsy surgery is done and sent out for a microscopic pathological exam.
Also, various periodontal surgeries are many times indicated for later stage gum disease.
What Are Wisdom Teeth?
Your wisdom teeth are your third set of molars; the ones all the way at the back of your mouth. They generally try to erupt between the ages of 17 to 21 years, and, since that is apparently when you supposedly become “wise”, we thus have the term “wisdom teeth.”
Although they are the last teeth to appear in your mouth, they are really no different and can be just as useful as than any other teeth.
However, in most mouths, there is insufficient space for them, so many problems can arise.
Benefits of Wisdom Teeth Removal
Do Wisdom Teeth Have To Come Out?
Yes — for the overwhelming majority of people.
No — for a very small number who have smaller teeth in general, a larger jaw or their wisdom teeth erupt properly.
Wisdom teeth can be quite a problem for many people. Usually around age 18 to 20 they erupt and cause pain, infection or a painful pressure sensation. They are sometimes guilty of damaging nearby teeth or even forming cysts or tumors in the area. Gum disease will thrive in areas that cannot be properly cleaned, whether erupted or not.
In addition to problems with infection, the pressure from their eruption leads to increased crowding in the mouth. Wisdom teeth are seldom straight enough to help in chewing, and for most people, removal is the best option. That is what I have done for myself and all of my family.
Rarely is someone seen with useful wisdom teeth, and, of course, in that case they should be left alone and kept healthy. A special 3D x-ray scan will usually be all that is needed to properly evaluate whether or not extractions are needed.
If so, luckily hospitalization and general anesthesia are usually NOT needed for this procedure. Great outcomes, at lowered expense and risk can be obtained by using only mild sedation and local anesthesia. This is how we routinely do this surgery at our clinic. You usually do not even have to have someone come drive you home unless you desire.
Can I Wait To Get My Wisdom Teeth Out?
If your wisdom teeth are not causing you any problems at the moment, sure you can wait… but (and that’s a big “but”) there are several things you should consider:
What are the chances that you will never have any problems with your wisdom teeth? (Hint: quite small)
Having your wisdom teeth removed is rarely harmful to your health.
Skipping hospitalization and general anesthesia means lower risk AND lower cost.
Generally the younger you are, the easier the surgery, because the roots of the teeth are not fully developed and the jawbone is not as dense. The easier it is to remove your wisdom teeth, the easier your recovery will most likely be.
If you are older than age 30 and still have your wisdom teeth, there is probably only a small risk of them causing problems in the future, IF you are cleaning the area properly.
If you have a chronic medical condition that could worsen, it may be best to have your wisdom teeth removed sooner rather than later. Wisdom teeth surgery could affect your medical condition and visa versa.
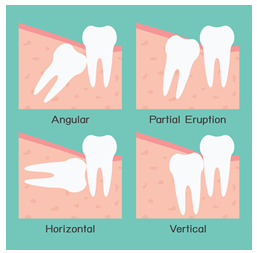
By opting to get your wisdom teeth out sooner, you can avoid many complications caused by impacted ones, those that are still stuck in the jaw and haven’t properly broken through the gums.
Gum disease and decay is common in the area of wisdom teeth and their removal can also lessen the chances of infection, cysts and tumors.
FAQ About Wisdom Teeth?
How bad is this going to hurt?
It varies widely due to many factors, but most of my patients are back to 100% chewing and feeling good after about 5-6 days.
Of course, complicating factors can lengthen this, but also there some patients who can hardly tell it’s been done after only 3 days!
During the procedure we try to make sure you have no pain, but then the most important time is after the surgery. We give you oral and written instructions on what to do and not do.
The most common complication is due to poor post-operative follow through, but don’t worry! I routinely call all of my surgical patients the evening after their dental visit to check up on them and answer any questions or concerns they might have.
My friends and family say this is an awful procedure. What do I do?
Well, you just need a little better advice coming your way! If we use proper technique and you manage good post-operative follow through, then problems like severe pain and swelling are fairly rare in our office — probably less than 5%!
I want to be put to sleep. Isn’t that the best way?
Of course it is your choice, but light sedation with local anesthesia is not only less expensive, it’s safer and easier. If you are “put to sleep” for the procedure, there are additional risk factors and you are unable to drive yourself home.
What Is Oral Bone Grafting?
Being able to add bone in a needed area of the body is a good thing, and is used by different doctors to help different areas of our bodies. In the mouth, bone grafting is used primarily in tooth extraction sockets, in preparation for dental implants or to aid implant placement.
After teeth are extracted, oftentimes the surrounding bone will shrink considerably, up to 50% of the former volume in the area. The body resorbs this bone because the tooth is gone and the bone won’t be needed.
However, bone shrinkage is a bad thing because original jaw structure and facial structure can be altered irreversibly. Bone grafting after an extraction basically entails placing some type of additional bone (usually a synthetic bone mineral with a sand-like texture) in the empty socket and carefully covering and suturing it in so it will “take”. The body will usually accept the new tissue and new bone cells will form throughout the graft and totally integrate within a few months. This can form a much more stable and strong base to place dental implants.
In years past, if a patient had excessive bone resorption, implants were many times impossible. Now we can anticipate the shrinkage, and place the proper socket bone graft at the time of the extraction. Even if the final plan is not for implants, a preserved ridge is a better foundation for any type of bridge that could be used to replace the tooth.
What Is A Frenectomy?
Let’s start with, “What is a frenum?”
A frenum, also called a frenulum, is a thin fold of mucous membrane with a few enclosed muscle fibers that can be found in various areas inside the mouth. If you run the tip of your tongue over your two upper front teeth and up toward your nose, you will most likely find a frenum.
Likewise, if you do the same over your lower two front teeth and down toward your chin, you will find another frenum connecting your gum to your inner lip. If you touch the roof of your mouth with your tongue while looking in a mirror, you will probably notice another frenum connecting the bottom of your tongue to the bottom of your mouth.
A frenectomy is simply a surgical procedure to remove one of these frenums.
These muscle attachments usually cause no problems, but occasionally, when a frenum is too tight, in the wrong place or causes undesirable forces on gums or teeth, a frenectomy is done.
For instance, some people have a tight frenum under the tongue that limits movement and affects eating and speech. In this case, we say the person is “tongue-tied.”
Another effect is when a frenum pulls on the area between your two front teeth. During orthodontic treatment, this may actually inhibit the closure of the gap between those teeth.
Frenums can even interfere with the fit of your denture.
In our office, we have found frenectomies performed with a laser to be the best for our patients. The controlled delivery of laser energy generally means our patients experience minimal trauma to the surrounding tissues, less bleeding, little or no pain and quicker healing time.
